Hepatitis
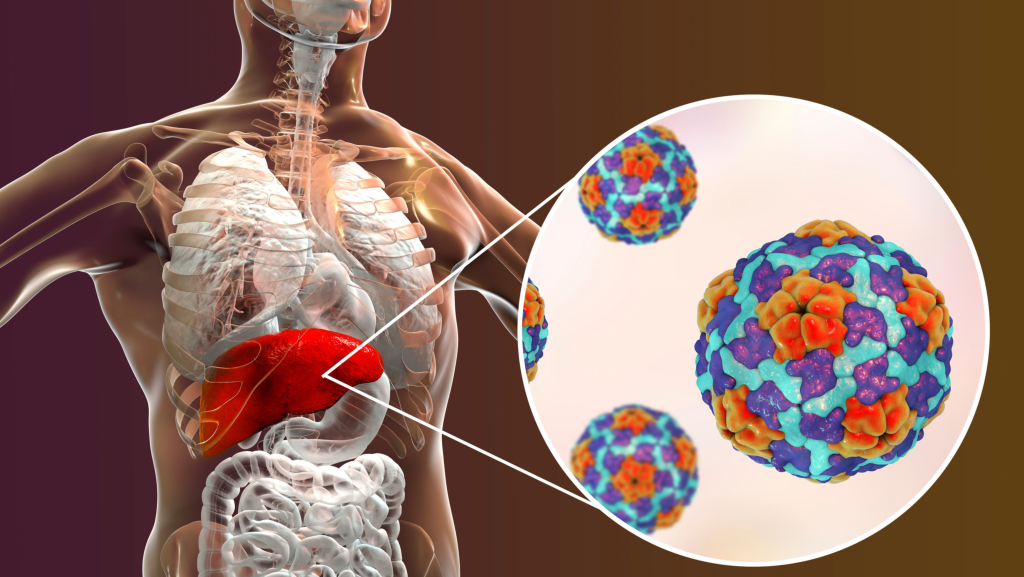
Hepatitis: Types, Symptoms and Prevention Hepatitis is an inflammation of the liver, an organ vital for metabolism, detoxification, and protein production. It can be caused by viruses, toxins, or autoimmune factors and can be acute or chronic, sometimes leading to serious complications such as cirrhosis or liver cancer. Main Types of Hepatitis Hepatitis is mainly divided into several types, the most common of which are viral: Hepatitis A: Caused by the HAV virus and spread through food, water, or contact with infected people. It is usually mild and goes away on its own. Hepatitis B: It is caused by the HBV virus and is transmitted through blood, sexual intercourse or from mother to child. It can become chronic and dangerous for long-term health. Hepatitis C: Caused by the HCV virus and transmitted primarily through exposure to infected blood. It often becomes chronic and can lead to serious complications. Hepatitis D: Requires the presence of the HBV virus and is the most dangerous of the viral hepatitis. Hepatitis E: It is transmitted mainly through contaminated water and is more common in regions with poor sanitation. Hepatitis can also be caused by: Excessive alcohol consumption Exposure to toxic substances Autoimmune diseases Symptoms of Hepatitis Many people with hepatitis have no symptoms in the early stages. When they do appear, they include: Constant tiredness Jaundice: Yellow Skin and Eyes Dark urine and light stool Pain in the upper right part of the abdomen Nausea, vomiting and loss of appetite Diagnosis and Treatment Diagnosis Blood tests to detect viruses and evaluate liver function In special cases, a liver biopsy may be necessary. Treatment Hepatitis A and E: Most cases are treated with rest, hydration, and a healthy diet. Hepatitis B and C: Antiviral drugs are used to reduce viral load and prevent liver damage. Autoimmune hepatitis: Corticosteroids and immunosuppressants help control inflammation. Hepatitis Prevention Prevention is essential to avoid hepatitis: Vaccination: Vaccination against hepatitis A and B is effective and widely recommended. Hygiene: Wash your hands regularly and avoid contaminated food and water. Sexual safety: Use protection to avoid HBV and HCV. Avoid sharing personal items: needles, razors and toothbrushes. Conclusion Hepatitis is a disease that affects millions of people worldwide. Awareness, early diagnosis and proper care are important for treatment and prevention. With the right measures, many cases can be successfully managed or even avoided altogether. Take care of your health and contact a doctor for any liver-related problems! Together for a healthy future! Book your consultation with a specialist doctor now! Your Medical Clinic staff provides all patients with specialized medical service at the highest standards. (+355) 69 627 7162
Anemia EN
What is Anemia? Anemia is a medical condition that occurs when the body does not have enough red blood cells or hemoglobin to carry oxygen to the tissues. This can cause tiredness, weakness, and other symptoms that affect the quality of life. Anemia is one of the most common health problems in the world, affecting people of all ages and genders. Main causes of anemia Anemia can have different causes and types. Some of the main factors include: Iron Deficiency (Iron Deficiency Anemia)Caused by a diet low in iron, blood loss (e.g. during heavy menstruation or gastrointestinal bleeding) or poor iron absorption. Vitamin B12 and Folic Acid DeficiencyThese nutrients are essential for the production of red blood cells. Their deficiency can cause megaloblastic anemia. Chronic DiseasesConditions such as diabetes, kidney disease, or chronic inflammation that inhibit the production of red blood cells. Hemolytic AnemiaRed blood cells are destroyed faster than the bone marrow can produce them. Genetic DiseasesDiseases such as sickle cell anemia or thalassemia that affect the shape and function of red blood cells. Heavy Blood LossTrauma, surgery, or heavy menstrual periods can cause this condition. Cases of MalabsorptionPathologies such as Crohn’s disease or celiac disease prevent the absorption of nutrients. Symptoms of Anemia Symptoms vary depending on the type and severity of anemia. Some of the most common are: Tiredness and weakness Yellowing of the skin and mucous membranes Dizziness or feeling faint Difficulty breathing, especially during physical activity Rapid or irregular heartbeat Headache and poor concentration Cold hands and feet Weak nails and hair loss Caution: If you experience these symptoms for a prolonged period, consult a doctor to determine the cause and adopt the most appropriate treatment. Diagnosis of Anemia The diagnosis is made through: Blood test (CBC): Evaluates the levels of hemoglobin and red blood cells Lab tests: Measure levels of iron, vitamin B12 and folic acid Hemoglobin electrophoresis: For the diagnosis of thalassemia and genetic diseases Coombs test: Identify autoimmune hemolytic anemias Treatment of Anemia Treatment is determined by the cause of the anemia: Iron DeficiencyIron supplements and inclusion of foods such as red meat, spinach and fortified cereals. Vitamin B12 and Folic Acid DeficiencyOral supplements or injections of vitamin B12 and folic acid. Foods such as eggs and dairy products may also help. Anemia of Chronic DiseaseTreatment of the underlying disease; in more severe cases, blood transfusions or erythropoietin injections. Hemolytic Anemia or Genetic DisordersBlood transfusions, immunosuppressant drugs, or bone marrow transplants may be necessary. Prevention of Anemia Include foods rich in iron, vitamin B12 and folic acid in your diet Use food supplements when necessary, especially during pregnancy or in the presence of risk factors Maintain a healthy lifestyle and undergo regular medical check-ups Conclusion Anemia is a condition that can significantly impact your quality of life. However, with early diagnosis and proper treatment, it is manageable and preventable.Take care of your health and don’t ignore the signs of anemia. Together for a healthy future! Book your consultation with a specialist doctor now! Your Medical Clinic staff provides all patients with specialized medical service at the highest standards. (+355) 69 627 7162
Gastroscopy

Gastroscopy Gastroscopy: What You Need to Know Gastroscopy is a procedure in which a specialist looks inside the upper digestive tract. In this procedure, the esophagus, stomach, and duodenum (small intestine) are examined using an instrument called a gastroscope. What is Gastroscopy? The gastroscope is a thin, flexible instrument, thinner than your little finger. It passes through the mouth, through the esophagus, into the stomach, and reaches the beginning of the duodenum. It has a camera and a light at the end. In addition, an internal channel allows the passage of auxiliary instruments for the examination, such as thin forceps or loops for the removal of foreign bodies. When is it necessary to undergo a gastroscopy? Gastroscopy may be necessary in the following cases: Reflux of gastric juices into the esophagus Burning behind the sternum Pain in the upper abdomen Frequent vomiting Difficulty swallowing These symptoms may indicate: Gastroesophageal reflux (GERD) Esophagitis Duodenal or gastric ulcer Duodenitis (inflammation of the duodenum) Gastritis (inflammation of the stomach) Stomach or esophageal cancer How is a Gastroscopy Performed? The gastroscopy procedure usually takes about 15 minutes, including preparation and sedation time. It is not painful, but may cause slight discomfort as the stomach is inflated with air for a clearer view. What Instructions Should I Follow Before the Procedure? The stomach must be empty, so the patient should not eat for at least 8 hours before the examination. Sedation (calming) may be necessary, so it is recommended that you bring someone with you. It is recommended to stop taking certain medications, such as anticoagulants, 1-2 days before the procedure. How is Gastroscopy Tolerated? Many patients have misinformation and perceive it as a difficult procedure that causes anxiety. In reality, it is the opposite: it is a simple, painless and safe procedure. It is one of the most important tests to establish a correct diagnosis and guide treatment. After the examination, the patient can leave the clinic and go home within 30–60 minutes. If sedation has been administered, you may need to stay in the clinic longer. After exiting, you should not drive for 2 hours, operate machinery for 2 hours, or consume alcohol for 24 hours. It is important to be accompanied. Should Gastroscopy Be Repeated? After treatment, a follow-up visit is usually recommended to reassess the condition. Together for a healthy future! Book your consultation with a specialist doctor now! Your Medical Clinic staff provides all patients with specialized medical service at the highest standards. (+355) 69 627 7162
Ulcers

Ulcers What are ulcers? Gastric and duodenal ulcers are a common condition in clinical patients. The best method to diagnose them is video endoscopy of the upper digestive tract (gastroscopy), in which the doctor uses a thin tube with a camera to observe the lining of the stomach. Symptoms of ulcers Symptoms of ulcers can vary significantly from patient to patient. Some ulcers are painless, while others can be severe enough to disturb sleep. Common symptoms include: Abdominal pain Vomit Nausea Constipation or diarrhea Diagnosis and differential diagnosis Diagnosing ulcers requires ruling out other conditions such as gastritis, abdominal wall problems, and biliary tract disease. It is important to note that ulcers are curable with proper treatment. Complications The most common complications of ulcers include: Hemorrhage: One of the most common causes of gastric bleeding, with symptoms such as bloody vomiting and dark stools. The mortality rate for ulcerative hemorrhages remains high, around 7-10%. Perforation: Occurs when the ulcer ruptures, causing gastric contents to leak into the abdomen. This is an emergency situation that requires surgery. Penetration: An ulcer that penetrates the intestinal wall without causing rupture. It can lead to complications such as visceral abscess and hemorrhage. Obstruction: More rare, often associated with duodenal ulcers, it can block the normal passage of food. Diagnosis of Helicobacter pylori There is a strong link between Helicobacter pylori infection and the development of ulcers. Testing for this bacterium is standard for all patients with peptic ulcer disease. Treatment Treatment of ulcers includes: Appropriate treatment for one or more months Discontinuation of use of nonsteroidal anti-inflammatory drugs Continuous monitoring of symptoms to prevent complications Ulcers are curable, and with proper care, patients can recover completely. Together for a healthy future! Book your consultation with a specialist doctor now! Your Medical Clinic staff provides all patients with specialized medical service at the highest standards. (+355) 69 627 7162
Esophageal Cancer

Esophageal Cancer What is the esophagus? The esophagus is a muscular tube in the chest that is about 25 cm long. It helps food pass from the mouth to the stomach. The walls of the esophagus have four main layers: Inner layer : moist, which helps food slide easily into the stomach. Submucosa : Layer containing glands that produce mucus, keeping the esophagus moist. Muscle layer : Muscles help push food toward the stomach. Outer layer : covering that maintains the structure. Esophageal Cancer Facts The exact causes are unknown, but certain factors increase the risk. The risk increases with prolonged irritation of the esophagus, such as from smoking, alcohol, or Barrett’s esophagus. Cancer is diagnosed through barium tests and confirmed by endoscopy and biopsy. It can cause pain and difficulty swallowing. Treatment depends on the size, location, and extent of the tumor, as well as the patient’s age. Tumor cells Cells are the basic unit of tissue. Healthy cells grow, divide, and die. Sometimes, this process goes awry and unnecessary cells form, creating a tumor. Benign tumors : They are rarely life-threatening. They can be removed and are unlikely to grow back. They do not invade nearby tissues. Malignant tumors (cancer) : They can be life-threatening. They may grow back after removal. They invade and damage surrounding tissues and organs. They can spread to other parts of the body (metastasis). Esophageal cancer usually begins in the cells of the inner lining and can penetrate deep through the various layers of the esophagus. Types of Esophageal Cancer Adenocarcinoma : in the lower part of the esophagus, near the stomach. Squamous cell carcinoma : in the upper part of the esophagus. Risk factors Age : highest risk over 65 years. Gender : More common in men. Smoking : significantly increases the risk. Alcohol : especially if combined with smoking. Diet : low in fruit and vegetables. Obesity : linked to adenocarcinoma. Gastroesophageal reflux : can damage tissues. Barrett’s esophagus : It changes the cells, increasing the risk. Symptoms Esophageal cancer often does not show early signs. Over time, the following may appear: Regurgitation of food. Pain when swallowing. Chest or back pain. Weight loss. Burning. Hoarseness persisting for more than two weeks. These symptoms can also be caused by other, less serious disorders. Diagnosis Your doctor may recommend the following tests: Barium esophagoscopy : visualization using contrast medium. Endoscopy : exploration with a flexible instrument (gastroscope). Biopsy : sampling of tissue for analysis. Staging After diagnosis, the extent of the cancer’s spread is assessed to decide on the appropriate treatment: Depth of the tumor. Involvement of nearby tissues. Spread to other organs. Cancer stages : Stage 0 : Abnormal cells only in the inner layer. Stage I : penetrates the submucosa. Stage II : Involves lymph nodes and deeper layers. Stage III : Reaches the outer layer and nearby organs. Stage IV : It has spread to other organs (metastasis). Treatment Options include: Surgery Radiotherapy Chemotherapy The choice depends on: Location of the tumor. Extension and diffusion. General condition of the patient. A multidisciplinary team is needed to personalize the treatment plan. Useful questions to ask your doctor What is the stage of the disease? Has the cancer spread? What is the goal of therapy? What are the treatment options available? This is a serious condition. Being informed will help you make clear decisions about your health. Together for a healthy future! Book your consultation with a specialist doctor now! Your Medical Clinic staff provides all patients with specialized medical service at the highest standards. (+355) 69 627 7162
Pink October at Your Medical Clinic

Pink October Breast Cancer Awareness Month at the YMC October is a special month dedicated to raising awareness about breast cancer and encouraging early screening.Each year, this month reminds us of the importance of taking care of our health and taking proactive steps to prevent and detect serious diseases early. What is Pink October? Pink October is a global campaign that aims to raise awareness of breast cancer, one of the most common diseases among women.During this month, hospitals and health organizations around the world are committed to educating women and men about the importance of early diagnosis, effective treatments, and support for those affected by this disease. The Importance of Early Screening In our hospital, we emphasize that early screening can be a crucial factor in the fight against breast cancer.Ultrasound, clinical examination and breast self-examination are essential to detect any changes in the early stages.Early diagnosis significantly increases the chances of successful treatment and complete recovery. What Can You Do? During this month, we invite you to have routine checkups at our hospital, where our specialized staff will take care of you with professionalism and dedication.In addition to ultrasound, we also offer consultations to learn more about methods of prevention and treatment of breast cancer. Our Hospital Services during Pink October As part of the Pink October campaign, our hospital offers you: Ultrasound and specialist tests Consultations with oncologists Lifestyle and risk factor reduction counseling Psychological support for patients and their families Breast health is a responsibility we must take seriously.Don’t postpone your check-up and take advantage of the services offered during Pink October.Together we can take important steps towards preventing and fighting breast cancer. Together for a healthy future! Book your consultation with a specialist doctor now! Your Medical Clinic staff provides all patients with specialized medical service at the highest standards. (+355) 69 627 7162
Irritable Bowel Syndrome

What is Irritable Bowel Syndrome? Irritable bowel syndrome (IBS) is one of the most common intestinal disorders, affecting millions of people worldwide. Although it is not a life-threatening condition, its symptoms can be difficult to manage and have a significant impact on an individual’s quality of life. In this blog, we will look at what irritable bowel syndrome is, its main symptoms, causes, and ways to manage it. What causes irritable bowel syndrome? Irritable bowel syndrome (IBS) is a functional bowel disorder, meaning there is no apparent structural problem, but it is related to a dysfunction of the digestive system. Key factors include: Changes in intestinal motility: rapid or slow movements, causing diarrhea or constipation. High intestinal sensitivity: more pronounced pain due to different processing of signals by the brain and nervous system. Stress and Anxiety: Psychological Factors That Negatively Affect the Brain-Gut Connection. Gut Microbiome Changes: An Imbalance of Beneficial Bacteria in the Gut. Main symptoms of irritable bowel syndrome Symptoms of irritable bowel syndrome vary from person to person, but some of the most common include: Abdominal pain or cramps: These usually subside after a bowel movement. Bloating and gas: Feeling bloated after eating. Changes in bowel movements: alternating between diarrhea and constipation. Sensation of incomplete defecation: after going to the bathroom. Mucus in stool: A common sign in some individuals. How is irritable bowel syndrome diagnosed? The diagnosis of irritable bowel syndrome excludes other intestinal diseases. The diagnostic process includes: History and symptoms: to identify patterns and causal factors. Blood and stool tests: to rule out food intolerances or infections. Endoscopy or colonoscopy: in severe cases or with unusual symptoms. Treatment Options for Irritable Bowel Syndrome Managing irritable bowel syndrome requires a combined approach through lifestyle changes, diet and sometimes medications: Dietary changes Try the low FODMAP diet to reduce symptoms. If you suffer from constipation, gradually increase your fiber intake. Avoid common triggers, such as caffeine and spicy foods. Stress Management Relaxation practices such as meditation, yoga, and deep breathing. Cognitive behavioral therapy (CBT) to manage emotional stress. Medicines and supplements Antispasmodics to relieve pain. Probiotics to improve the gut microbiome. Specific medications for constipation or diarrhea. How to live with irritable bowel syndrome? Improving your quality of life is possible with proper management. Keep a food diary to identify triggers, eat regularly, and stay hydrated. Conclusion Irritable bowel syndrome can be a difficult condition to manage, but with the right medical support and an integrated approach to management, most patients can live full, active lives. If you think you may have irritable bowel syndrome, consult a specialist to develop a personalized treatment plan. Together for a healthy future! Book your consultation with a specialist doctor now! Your Medical Clinic staff provides all patients with specialized medical service at the highest standards. (+355) 69 627 7162
Pancreatitis

What is pancreatitis? Pancreatitis is an inflammatory disease of the pancreas, a small but vital organ located behind the stomach that plays an important role in digestion and blood sugar regulation. Inflammation can occur in acute, chronic, or autoimmune forms and can sometimes lead to serious complications. Types of Pancreatitis 1. Acute Pancreatitis • It appears suddenly and lasts a few days.• In most cases it is mild, but in severe cases it can be life-threatening. 2. Chronic Pancreatitis • It develops due to repeated inflammation, causing permanent damage.• It is often associated with prolonged alcohol consumption. 3. Autoimmune Pancreatitis • A rare form caused by the immune system.• It is mainly treated with corticosteroids. Main Causes of Pancreatitis • Gallstones: These block the pancreatic duct and cause inflammation.• Excessive alcohol consumption: A common cause of both acute and chronic forms.• Drugs: Some medications can cause side effects that affect the pancreas.• Abdominal infections and trauma: Physical injuries or viral infections can cause inflammation.• Genetic factors: Some forms are linked to inherited diseases such as cystic fibrosis. Symptoms of Pancreatitis • Severe abdominal pain radiating to the back.• Nausea and vomiting, especially after meals.• Loss of appetite and body weight.• Fever and general weakness.• Fatty, pale stools due to lack of digestive enzymes. Diagnosis of Pancreatitis • Blood tests: Measurement of lipase and amylase levels.• Ultrasound, ultrasound, and MRI: To evaluate inflammation or damage to the pancreas.• Endoscopy: To identify gallstones or problems with the pancreatic ducts. Treatment of Pancreatitis 1. Acute Pancreatitis • Intravenous hydration and pain control.• Treatment of gallstones if they are the cause.• Soft diet for the pancreas until improvement. 2. Chronic Pancreatitis • Use of digestive enzymes to improve digestion.• Pain management with medications or nerve blocks.• Lifestyle changes, avoiding alcohol and heavy foods. 3. Autoimmune Pancreatitis • Corticosteroids to control inflammation and damage. Prevention of Pancreatitis • Avoid alcohol and smoking: The main risk factors.• Control of gallstones: Their treatment prevents acute pancreatitis.• Healthy diet: Diet rich in fiber and low in fat.• Control of cholesterol and triglyceride levels: To protect the pancreas. Conclusion Pancreatitis is a serious condition that requires timely attention and specialized treatment. If you experience severe abdominal pain or other symptoms, contact your doctor immediately. Timely treatment is essential for successful recovery and maintaining the health of your pancreas. Together for a healthy future! Book your consultation with a specialist doctor now! Your Medical Clinic staff provides all patients with specialized medical service at the highest standards. (+355) 69 627 7162
Epilepsy
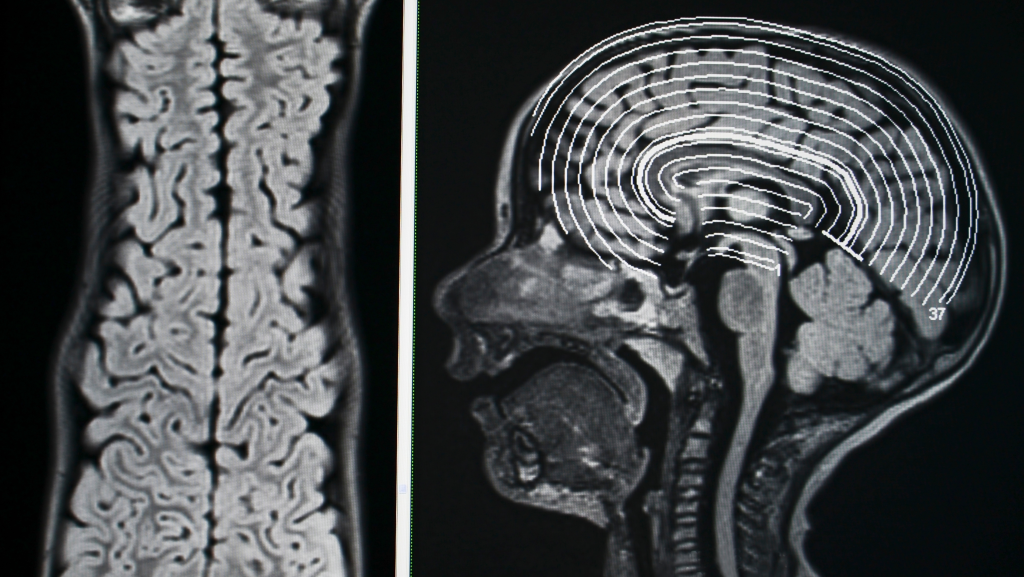
What is Epilepsy? Epilepsy is a group of neurological disorders characterized by recurrent and unprovoked seizures. It can affect people of any age, gender, or ethnicity, but the causes are often varied and, in some cases, unknown. Main Causes of Epilepsy Epilepsy can be caused by many factors, including: Brain damage Head trauma due to accidents or injuries. Stroke, including hemorrhage and ischemia. Neurological diseases Brain infections, such as meningitis or encephalitis. Brain tumors. Genetic factors Specific mutations associated with inherited forms of epilepsy. Developmental Disorders Autism and other developmental disorders. Other causes Lack of oxygen during childbirth. Use of toxic substances or withdrawal from drugs and alcohol. Types of Epileptic Seizures Epileptic seizures are divided into two main categories: Partial seizures They originate in a part of the brain and cause symptoms such as unusual sensations, confusion, or uncontrolled movements. Generalized crises They involve the entire brain and are often accompanied by loss of consciousness. The most common types include: Tonic-clonic seizures : tremors and stiffening of the body. Absence seizures : brief disconnections from reality. Myoclonic seizures : sudden muscle contractions. Main Symptoms of Epilepsy Epilepsy presents with a variety of symptoms including: Sudden loss of consciousness. Uncontrolled tremors. Temporary disconnection or confusion. Unusual sensations ( aura ), such as strange sounds or smells. Diagnosis of Epilepsy The diagnosis of epilepsy is made by a neurologist and includes: History and description of convulsive seizures. Electroencephalogram (EEG) to record electrical activity in the brain. Imaging tests , such as MRI or CT scan, to detect damage. Blood tests to rule out metabolic causes or infections. Treatment of Epilepsy Although there is no cure, treatment can effectively manage the condition. The main options include: Antiepileptic drugs (AEDs) They prevent seizures if taken as directed by your doctor. Surgery In special cases, the part of the brain that causes the seizures is removed. Vagus nerve stimulation (VNS) A device that helps manage crises. Lifestyle changes Avoid stress and fatigue and, when necessary, follow a ketogenic diet. Daily Management Monitoring seizures : Keep a diary to identify triggers. First Aid : Ensuring a Safe Environment During Crises. Psychological support : Consult a psychologist to deal with emotional challenges. Prevention of Complications Compliance with the therapies prescribed by the doctor. Avoid dangerous activities, such as swimming without supervision. Support from epilepsy communities and groups. Conclusion Epilepsy, despite the difficulties it can cause, is a manageable condition. Understanding it and receiving ongoing support from your doctors and family is essential for a healthy and productive life. Together for a healthy future! Book your consultation with a specialist doctor now! Your Medical Clinic staff provides all patients with specialized medical service at the highest standards. (+355) 69 627 7162
Osteoporosis
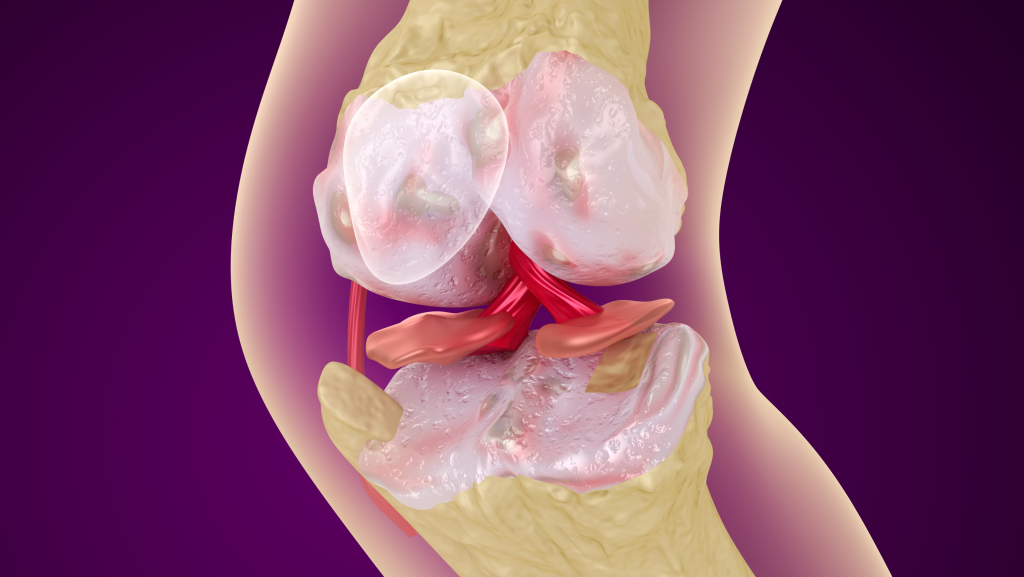
What is Osteoporosis? Osteoporosis is a disease in which bones lose density and strength, becoming more fragile and prone to fracture. This condition poses a serious challenge to bone health, especially as we age. Causes and Risk Factors 1. Non-modifiable risk factors: • Age: The risk increases with age. • Gender: Women are more predisposed due to hormonal changes after menopause. • Family history: A family history of osteoporosis increases the risk. 2. Modifiable risk factors: • Poor diet: Lack of calcium and vitamin D. • Sedentary lifestyle: Lack of physical activity damages bone strength. • Smoking and alcohol: Reduced bone density. • Medications: Some medications, such as corticosteroids, can damage bones. Symptoms of Osteoporosis Osteoporosis often develops silently without any obvious symptoms. However, symptoms may include: • Minor bone fractures, such as after a minor fall. • Reduction in height over time. • Back pain due to fractures of the vertebrae. • Stooped posture (kyphosis). Diagnosis of Osteoporosis The diagnosis is made with specific tests: • Bone densitometry (DXA): Test that measures bone mineral density. • Blood and urine tests: Evaluation of calcium and vitamin D levels. Osteoporosis Treatment Treatment aims to slow bone loss, strengthen existing bones, and reduce the risk of fractures. 1. Drug therapy: • Bisphosphonates: Drugs that slow the loss of bone density. • Denosumab: Injectable therapy that strengthens bones. • Hormones: Hormone therapy for women after menopause. 2. Diet and supplements: • Increase calcium and vitamin D intake through dairy products and fish. 3. Physical activity: • Weight-bearing exercises, such as walking, running, or lifting weights, help strengthen bones. 4. Lifestyle changes: • Avoid smoking and alcohol. • Make your home safe to reduce the risk of falls. Osteoporosis Prevention Prevention is essential! Some tips to protect bone health: • Balanced diet rich in calcium and vitamin D. • Regular physical activity to stimulate bone health. • Early screening for post-menopausal women and people at high risk. Osteoporosis is a common disease, but it can be managed and prevented with proper care. Together for a healthy future! Book your consultation with a specialist doctor now! Your Medical Clinic staff provides all patients with specialized medical service at the highest standards. (+355) 69 627 7162

