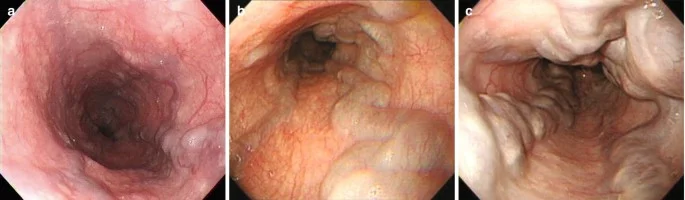
Barrett’s Esophagus
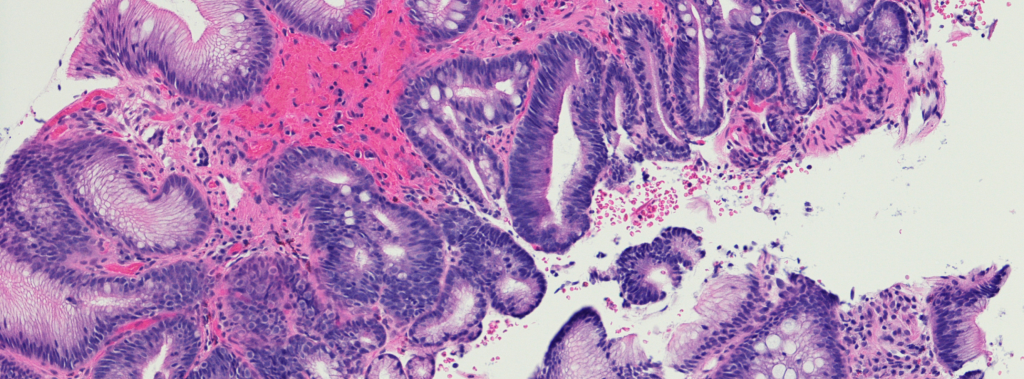
Barrett’s Esophagus Barrett’s Esophagus: A Detailed Review What is Barrett’s esophagus? Barrett’s esophagus is a condition in which the esophagus, the muscular tube that carries food and saliva from the mouth to the stomach, undergoes significant changes. Its normal lining is replaced by cells similar to those in the intestine. Although Barrett’s esophagus itself may not cause symptoms, it is closely linked to the risk of developing esophageal cancer, especially in people with gastroesophageal reflux disease (GERD). Normal esophageal function The esophagus has an important function: to transport food, liquids and saliva from the mouth to the stomach. The stomach functions as a sort of storage, where the digestion of food begins, which is then sent to the intestine for further digestion. Digested food is absorbed by the intestine through a process called peristalsis, which is imperceptible to us. When these contractions are intense, they can cause discomfort, especially if hot or cold solid foods or liquids are ingested. Sphincter mechanisms The muscular layers of the esophagus are narrowed at both ends by circular muscles called “sphincters.” When a person swallows, the sphincters relax to allow food to pass through. After passage, the sphincters close to prevent food from flowing back into the esophagus and into the mouth. A phenomenon known as reflux occurs when the sphincters relax and a small amount of food or liquid flows back into the esophagus. What is GERD? Gastroesophageal reflux disease (GERD) occurs when stomach acid frequently backs up into the esophagus. Although it does occur sometimes, frequent and uncontrolled reflux is a sign of a health problem that requires medical attention. Typical symptoms include heartburn and may be caused by obesity, certain foods, or pregnancy. Reflux and Barrett’s Esophagus Although the exact cause of Barrett’s esophagus is unknown, reflux is thought to play a role. Barrett’s esophagus is more common in men and whites, and is relatively rare in children. Cancer Risk Barrett’s esophagus is a precursor to esophageal adenocarcinoma. The risk of developing cancer is 30 to 125 times higher in people with Barrett’s esophagus than in those without the disease. The increase in esophageal adenocarcinoma is linked to obesity and gastroesophageal reflux. troubleshooting Barrett’s esophagus can only be diagnosed by endoscopy (gastroscopy). During this procedure, your doctor may perform a biopsy if suspicious mucus is noted. Patients over age 40 with GERD are recommended to have an endoscopy every two years to monitor changes. Treatment There is no drug cure for Barrett’s esophagus. Surgical removal of the affected area is an option, especially for patients at high risk of cancer. Many specialists recommend treatment of gastroesophageal disease, but this measure does not guarantee prevention of cancer development. Observation for dysplasia and cancer Periodic endoscopies are important to monitor changes in patients with Barrett’s esophagus. If dysplasia develops, the process must progress to an intermediate stage where cancer cells appear in the esophageal tissue, and this is only confirmed by biopsy. Important research questions There are several areas that require further study, including: Method for identifying individuals with problems. Causes of Barrett’s esophagus. Treatments to prevent or eliminate it. Optimal treatments for patients with Barrett’s esophagus or cancer. Conclusion Some important things to remember are: In Barrett’s esophagus, the cells change and become similar to those in the intestine. It is closely related to GERD. A small number of patients with Barrett’s esophagus may develop esophageal cancer. Diagnosis is made through endoscopy and biopsy. Patients are advised to undergo periodic endoscopy. Taking antacids can help, but should be done under the supervision of a doctor. Surgical removal is recommended only for patients at high risk of cancer. It is hoped that this information will help raise awareness of Barrett’s esophagus and the risks associated with it. Together for a healthy future! Book your consultation with a specialist doctor now! Your Medical Clinic staff provides all patients with specialized medical service at the highest standards. (+355) 69 627 7162
Ligation of Esophageal Varices
Ligation of Esophageal Varices Ligation of Esophageal Varices by Endoscopy Esophageal varices are abnormally dilated veins in the esophagus, characterized by very thin walls and high pressure inside them. This combination makes them very dangerous, as they can rupture and cause life-threatening bleeding. To treat these varicose veins, the varicose veins are ligated with rubber bands, a procedure performed through endoscopy, which is part of an upper gastrointestinal endoscopy. Reasons for the procedure This procedure is necessary to prevent or treat bleeding that can result from esophageal varices. If left untreated, they can rupture and cause severe bleeding. Possible complications Although complications following the procedure are rare, every procedure carries risks. Your doctor will consider the following options: Painful swallowing Bloodshed Esophageal damage Infection Some factors that may increase the risk of complications include: Alcoholism Bleeding disorders Active bleeding Old age Heart or lung problems Use of certain types of medications Tobacco What to expect? Before the procedure Your doctor will perform a physical exam and may order blood tests. Avoid eating for 8-12 hours before the procedure. If you have diabetes, talk to your doctor about any medications you should take. Arrange transportation, as you should not drive for 24 hours after the procedure. Talk to your doctor about any medications you are taking, as he or she may ask you to stop some for up to a week before the procedure. Anesthesia Local: You may be given a numbing solution to gargle with or a throat numbing anesthetic. Sedative: You may be given a sedative to help you relax. Conscious sedation: Drugs may be given intravenously to promote relaxation. General anesthesia: In case of uncontrolled bleeding, intubation and general anesthesia may be necessary. Description of the procedure To perform this procedure, you will be asked to lie on your left side. If intubation is not performed, a device will be placed to keep your mouth open. An assistant will monitor your breathing and heart rate. Oxygen may be given through your nose, and a tube will be used to remove saliva and other fluids. A lubricated endoscope will be inserted into your mouth and passed down your throat into your esophagus. The endoscope is equipped with a light and a camera, which allow the doctor to see images on a monitor. The doctor will fill the endoscope with air to see your esophagus more clearly and locate dilated veins. Instruments will be inserted into the endoscope and the enlarged tissue will be suctioned into the endoscopic device. One or more bandages will be placed around the tissue to help drain the blood. How many hours will it last? The procedure usually takes less than an hour. Will it be painful? During the procedure, you may feel pressure and discomfort, but not severe pain. Afterward, you may feel irritation and soreness in your throat. Post-procedure care At the treatment center After the procedure, you will be taken to a recovery room until the effects of the medication wear off. Most patients are kept under observation for about an hour and, if they feel well, can go home. At home After returning home, follow these tips: Follow your doctor’s dietary instructions. Avoid driving or operating heavy machinery for at least one day after the procedure. Avoid alcohol consumption for one day after the procedure. Make sure you get enough sleep. Over the days or weeks following surgery, the bandaged tissue will begin to come off. Continue to follow your doctor’s advice, as additional procedures may be necessary.Call your doctor Contact your doctor if you have: Signs of infection, including fever and chills Blood from the mouth Intensified pain Nausea and vomiting Vomiting blood Difficulty swallowing Cough, difficulty breathing or chest pain Confusion or weakness Bloody or very dark stools Severe abdominal pain Together for a healthy future! Book your consultation with a specialist doctor now! Your Medical Clinic staff provides all patients with specialized medical service at the highest standards. (+355) 69 627 7162
Achalasia
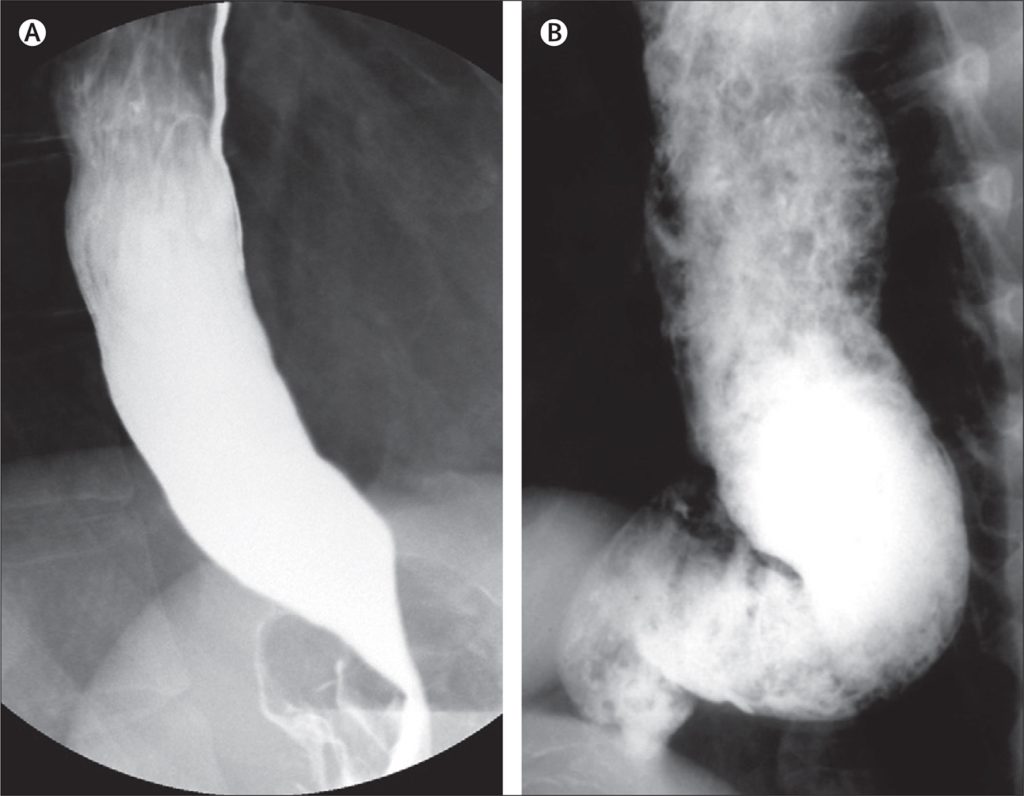
Achalasia Achalasia: A Complete Guide to This Rare Esophageal Disease What is achalasia? Achalasia is a rare disease that affects the muscles of the esophagus, the swallowing tube. The name “achalasia” means “inability to relax,” referring to the inability of the lower esophageal sphincter (the ring of muscle between the esophagus and the stomach) to open and allow food to pass into the stomach. This disability causes difficulty swallowing, causing significant discomfort in patients. How does the esophagus normally work? The esophagus is a complex structure composed of three functional parts: Upper esophageal sphincter: This sphincter, made up of ring-like muscles, separates the esophagus from the throat and remains closed most of the time, to prevent food from passing from the esophagus into the throat. Body of the esophagus: A muscular tube about 20 cm long that helps transport food to the stomach. Lower esophageal sphincter: Located at the end of the esophagus, this sphincter performs a similar function to the upper sphincter, preventing food and acidic stomach fluids from flowing back into the esophagus. During swallowing, the upper sphincter opens, allowing food and saliva to pass into the esophagus, while the esophageal muscles progressively contract to push food toward the stomach. How is achalasia diagnosed? Diagnosis of achalasia often begins with a review of the patient’s medical history. Common symptoms include dysphagia (difficulty swallowing), regurgitation of food, chest pain, and weight loss. These symptoms may worsen over time and often lead to a delayed diagnosis. Diagnostic methods X-ray: An examination using the contrast medium barium sulfate to visualize the esophagus. In achalasia, there is a dilation of the middle part of the esophagus and a characteristic narrowing of the lower part. Esophageal manometry: This test measures the pressure of the esophageal muscles during swallowing and helps identify abnormalities in muscle function. Endoscopy: A procedure that allows your doctor to look inside your esophagus and rule out other diseases, such as esophageal cancer. How is achalasia treated? Treatment of achalasia is multifactorial and includes several methods: Oral medications Oral medications such as nitrates and calcium channel blockers help relax the lower esophageal sphincter. However, these medications often provide temporary relief and may have side effects. Expansion Lower esophageal sphincter dilation is a procedure that involves the use of a balloon to dilate the sphincter. This procedure has a 60-95% success rate, but it can carry risks, such as tearing the esophagus. Surgery (Esophagomyotomy) Esophagomyotomy is a surgical procedure that involves cutting the lower esophageal sphincter to facilitate the passage of food. This procedure has a higher success rate than dilation, but does not guarantee a permanent cure. Botox Injection Botox injection into the lower sphincter is a nonsurgical option that provides relief for several months. It is a quick and safe procedure for elderly or high-risk surgical patients. Achalasia in brief Achalasia is a rare disease that affects the muscles of the esophagus and lower esophageal sphincter. The exact cause is unknown, but it is related to degeneration of muscle function. Symptoms include dysphagia, chest pain, and regurgitation. Treatment involves oral medications, dilation, surgery, and Botox injection. Achalasia requires a careful diagnostic and therapeutic approach to manage symptoms and prevent complications. If you experience swallowing-related symptoms, it is important to see a doctor for an accurate diagnosis and treatment. Together for a healthy future! Book your consultation with a specialist doctor now! Your Medical Clinic staff provides all patients with specialized medical service at the highest standards. (+355) 69 627 7162
Gastroesophageal Reflux
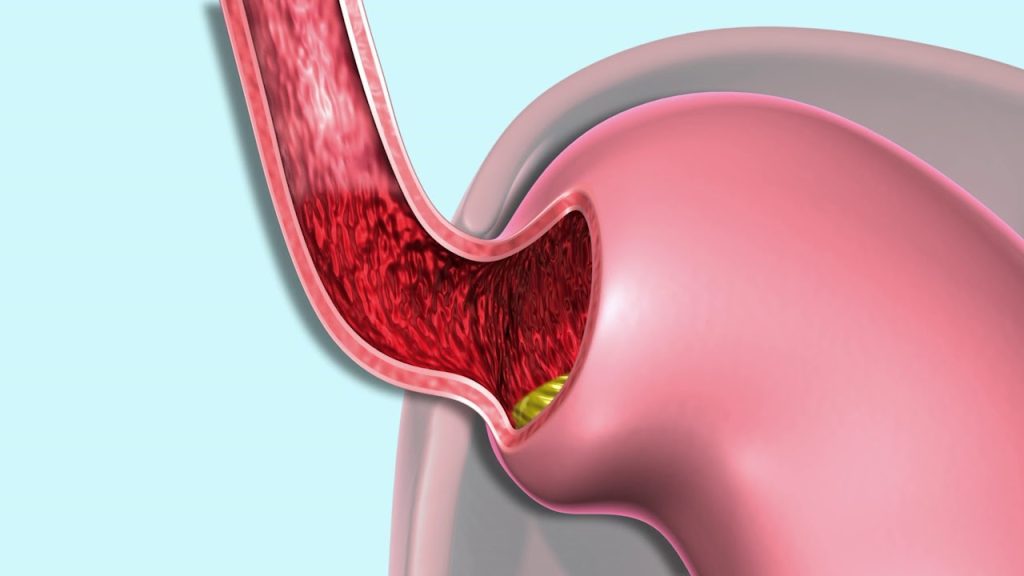
Gastroesophageal Reflux Gastroesophageal reflux in children and adolescents What is gastroesophageal reflux ? Gastroesophageal reflux occurs when stomach contents flow back into the esophagus during or after eating. The esophagus, which connects the mouth to the stomach, has circular muscles at the end that open and close to allow food to pass into the stomach. These muscles, known as the lower cardioesophageal sphincter (LESP), act as a valve at the entrance to the stomach. Reflux occurs when the LESP opens and allows acidic stomach contents to flow back up into the esophagus. This often begins in infancy, but most children outgrow it as they grow. What are the signs of gastroesophageal reflux? Most children and adults experience mild reflux, which often goes unnoticed. In cases where the regurgitated contents return quickly to the stomach, it does not damage the esophagus. In some cases, however, the acidic contents can remain in the esophagus and damage its lining, causing hoarseness or a chronic cough. Other signs include: Frequent pneumonia and bronchitis (due to aspiration of gastric juices). Respiratory difficulties. Difficulty or pain in swallowing. Vomit. Sore throat. Weight loss. Heartburn (more common in adults). Sensation of lump or tightness in the throat. How is gastroesophageal reflux diagnosed? To diagnose gastroesophageal reflux, you need to see a gastroenterologist. The doctor will ask you about your symptoms, perform a detailed physical exam, and recommend diagnostic tests. The most common tests to diagnose reflux are: Gastroscopy with contrast: This involves the collection of a barium fluid that helps visualize the damage and function of the esophageal sphincter and stomach through X-rays. Endoscopy (gastroscopy): This procedure involves the use of a flexible tube with a camera inserted through the mouth into the esophagus, stomach, and duodenum. The doctor may examine the lining and take a biopsy for further testing. Esophageal pH monitoring: A thin wire with an acid sensor is inserted to measure the amount of acidic fluid in the esophagus, helping to identify reflux during normal activities. What is the treatment for gastroesophageal reflux? Treatment depends on the symptoms of children and adults, with the aim of reducing the acidity of gastric juices. In addition to medications, it is important to follow some practical advice. For children: Frequent feeding in small quantities. Avoid eating 2-3 hours before going to bed. Raise the headboard of the bed a few centimetres. Avoid carbonated liquids and highly acidic foods. For adults: Smoking and alcohol consumption are prohibited. The use of chewing gum and mints is prohibited. Avoid stretching immediately after meals and eating late at night. Avoid wearing tight clothing and bending over after eating. Eat little and often. Lose weight if you are overweight. Keep the head of the bed a few inches higher. Avoid fatty and spicy foods, chocolate and fast food. Avoid citrus fruits and caffeine, which irritate the esophagus. Spicy and acidic foods can cause discomfort. If medications and dietary advice do not lead to improvement, surgery may be recommended, which is less common in children. Surgery involves fundoplication, a procedure that increases SPCE pressure and reduces the reflux of acidic fluids. What to keep in mind: Gastroesophageal reflux occurs when stomach contents flow back into the esophagus. It is a common problem in young children, but usually disappears as they grow. Treatment involves changes in diet and lifestyle, and surgery may be necessary if necessary. Together for a healthy future! Book your consultation with a specialist doctor now! Your Medical Clinic staff provides all patients with specialized medical service at the highest standards. (+355) 69 627 7162
Gastritis

Gastritis What is gastritis? Gastritis is an inflammation of the stomach lining. The term “gastritis” is often used improperly to include a series of disorders related to problems in the upper abdomen. In fact, it is an inflammation of the gastric mucosa, which can affect the entire mucosa or only a part of it. Gastritis can be classified as acute (immediate) or chronic. Acute gastritis can be erosive (with damage) or non-erosive. Chronic gastritis is diagnosed by histology (microscopic view of the mucosa). There are many causes of gastritis, but they often cause similar symptoms, which creates confusion. What causes gastritis? The main cause of both types of gastritis is infection of the gastric mucosa by the bacterium Helicobacter Pylori. This infection usually begins acutely in the antral region of the stomach and can develop over time throughout the stomach (chronic gastritis). Other causes include: Use of nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen. Bacterial, viral and parasitic infections. Alcohol Bile reflux. Fungal infections. Allergic reactions. Stress Trauma What are the signs of gastritis? Some patients have no symptoms and are diagnosed only by biopsy. When gastritis causes problems, signs include: Abdominal pain and burning. Nausea and vomiting. Diarrhea Loss of appetite. Gas All these symptoms are included in the term “dyspepsia”. How is gastritis diagnosed? Diagnosis of gastritis is made by clinical history, symptoms, and biopsy to identify the inflamed mucosa. The most common cause is Helicobacter Pylori, which can be identified with several tests. Endoscopic examination and biopsy also help identify chronic gastritis, erosions, and ulcers. Treatment of gastritis The most effective treatment is to address the causes. If the cause is Helicobacter Pylori, treatment is performed to eradicate it. If the triggers are nonsteroidal anti-inflammatory drugs, it is necessary to stop taking them. The rest of the treatment involves the use of antacids that reduce the production of gastric acid. What are the complications of gastritis? Over time, gastritis can lead to complications, especially if left untreated. These include: Peptic ulcer. Anemia Stomach cancer. Narrowing of the gastric lumen. The course of gastritis Some patients may recover quickly, especially those with mild disease. Patients with chronic gastritis or complications require ongoing treatment. How to prevent gastritis? If the cause is preventable, gastritis can be prevented. Limiting alcohol consumption and using anti-inflammatories carefully are excellent ways to reduce the risk. Proper hygiene and a healthy diet also help reduce the risk of infections. Together for a healthy future! Book your consultation with a specialist doctor now! Your Medical Clinic staff provides all patients with specialized medical service at the highest standards. (+355) 69 627 7162
Helicobacter Pylori EN
Helicobacter Pylori Helicobacter Pylori: What You Need to Know What is Helicobacter Pylori? Helicobacter pylori, also known as H. pylori, is a bacterium commonly found in the stomach that infects about half of the world’s population. Although many infected people have no symptoms, the bacterium can cause a variety of digestive tract problems, especially in the stomach and duodenum. It is not yet clear why some people develop problems related to the infection, while others remain asymptomatic. In this article, we discuss the symptoms, diagnosis, and treatment of H. pylori infection. Risk Factors and Transmission of H. Pylori pylori is mainly transmitted through contaminated food or water. The bacterium causes changes in the lining of the stomach and duodenum, producing enzymes and toxins that can damage the protective cells. This damage can lead to chronic inflammation (gastritis and duodenitis), making the stomach more vulnerable to gastric acid. The infection is very common in developing countries, including Albania, where children are often infected before the age of 10. Symptoms of H. Pylori Infection Many infected people have no symptoms, but when they do appear, they may include: Pain or burning in the upper abdomen Abdominal swelling Early feeling of satiety Loss of appetite Nausea or vomiting Dark or black stools (melena) In some cases, ulcers can cause bleeding, leading to anemia and fatigue. Chronic H. pylori infection may also increase the risk of stomach cancer, especially in areas where the infection is common since childhood. How is H. Pylori diagnosed? There are several methods to diagnose H. pylori, including: Blood test – Detects antibodies produced by the body against the bacteria. Breath test – A special test that detects the breakdown product of bacteria in exhaled air. Stool test – Detects the presence of the bacteria in the stool. Biopsy – During a gastroscopy, a sample is taken from the gastric mucosa and analyzed in a laboratory. Who should get tested for H. Pylori? The test is recommended for people with symptoms, active ulcers , or a history of ulcers . It may also be recommended for those with a family history of gastric cancer . Treatment of H. Pylori Gastric or duodenal ulcers associated with H. pylori infection should be treated. Treatment promotes healing and reduces the risk of recurrence and complications such as bleeding. Medications – Standard treatment involves a combination of medications taken for 7 or 14 days, such as: Proton pump inhibitors – Reduces acidity and helps the mucosa heal. Two antibiotics – Kill the bacteria and reduce the chance of resistance. Side effects of treatment About 50% of patients may experience mild side effects, while less than 10% discontinue treatment due to severe effects. The most common are: Metallic taste in the mouth Nausea, vomiting, headache Diarrhea or constipation Treatment failed Approximately 20% of patients do not clear the infection after the first course of therapy and may require a second treatment with different antibiotics. Summary pylori is a very common bacterium in the stomach. Although many infected people have no symptoms, it can cause stomach and duodenal ulcers and increase the risk of stomach cancer. Proper testing and treatment help treat the infection and prevent complications. After treatment, it is important to confirm eradication of the bacteria to ensure complete recovery. Together for a healthy future! Book your consultation with a specialist doctor now! Your Medical Clinic staff provides all patients with specialized medical service at the highest standards. (+355) 69 627 7162
Esophageal Varices: What You Need to Know
Esophageal Varices: What You Need to Know What are esophageal varices? Esophageal varices are abnormal dilations of veins that occur in the lower part of the esophagus, the tube that leads from the throat to the stomach. These veins often develop because of serious liver disease, which impedes the normal circulation of blood in this organ. As a result, blood backs up into smaller nearby veins, causing swelling and a high risk of bleeding. Esophageal varices often cause no symptoms until they begin to bleed. Because bleeding can be sudden and severe, it is critical to identify and treat the problem early. Bleeding can be life-threatening and requires immediate medical attention. Symptoms of esophageal varices Most people with esophageal varices have no symptoms until bleeding occurs. When this happens, the most common symptoms include: Hematemesis : Vomiting of blood, a symptom that requires immediate attention. Melena : Black, tarry stools, indicating the presence of digested blood. Abdominal pain : Abdominal pain or cramping may occur. Dysphagia and odynophagia : Difficulty and pain during swallowing. Confusion or lethargy : These may be signs of shock. Pallor : Indicates significant blood loss. Hypotension and tachycardia : Low blood pressure and rapid heartbeat. Reduced diuresis : Indicates impaired renal function. Causes of esophageal varices Varicose veins form when blood flow to the liver slows. This often happens because fibrotic tissue builds up in the liver, which increases pressure in the portal vein. The pressure pushes blood into smaller veins, causing them to dilate and increase the risk of rupture. Diseases that cause esophageal varices: Cirrhosis : Permanent liver damage, often caused by alcohol or hepatitis. Thrombosis : Blood clot in the portal vein or adjacent veins. Parasitic infections : E.g. schistosomiasis. Budd-Chiari syndrome : A rare condition resulting from clots in the liver veins. Risk factors Not all people with liver disease develop esophageal varices, but some factors increase the risk of bleeding: High pressure in the portal vein : The higher the pressure, the greater the risk. Large varicose veins : More likely to rupture. Red spots : Visible on endoscopy, they indicate high risk. Advanced cirrhosis or severe liver damage : Higher risk. Alcohol abuse : Aggravates liver damage. Complications Hemorrhage is the main complication of esophageal varices and can be fatal. In some cases, blood loss can lead to shock. Therefore, prevention and early diagnosis are essential. Diagnostics If you have cirrhosis or other serious liver disease, your doctor may recommend tests to identify esophageal varices, including: Endoscopy : Standard test to detect varices and risk of bleeding. Imaging techniques : CT, MRI or EUS to evaluate portal hypertension and other complications. Treatment The goal is to prevent bleeding. Treatment options include: Medicines : Beta-blockers such as nadolol or propranolol. Endoscopic procedures : Rubber band ligation or sclerotherapy. TIPS (Transjugular Intrahepatic Portosystemic Shunt) : Reduces pressure in the portal vein. Liver transplant : In the most severe cases and with recurrent bleeding. Prevention If you have liver disease, it is essential to take preventive measures: Avoid alcohol : It further damages the liver. Eat a healthy diet : Fruits, vegetables, whole grains; avoid fatty and fried foods. Control your weight : Being overweight worsens liver damage. Reduce your risk of hepatitis : Get vaccinated and follow safe practices Together for a healthy future! Book your consultation with a specialist doctor now! Your Medical Clinic staff provides all patients with specialized medical service at the highest standards. (+355) 69 627 7162
Thyroid Gland
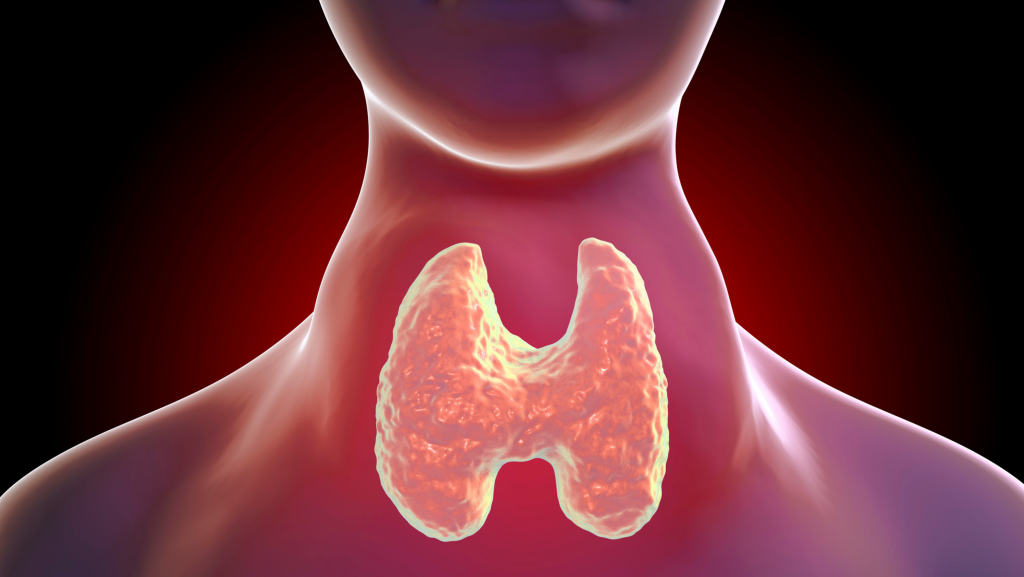
Goiter and everything you need to know What is Goiter and How is it Treated? The thyroid is a small, butterfly-shaped organ located in the front of the neck. This gland directly affects the metabolism and overall functioning of the body. One of the most common thyroid problems is goiter, an enlargement of the gland, which affects millions of people around the world. But what is goiter, why does it develop, and how can it be treated? What is Goiter? Goiter is an enlargement of the thyroid gland, which may or may not be visible. This condition may be associated with normal (euthyroidism), increased (hyperthyroidism), or decreased (hypothyroidism) thyroid function. Types of Goiter: Diffuse: When the entire gland is uniformly enlarged. Nodular: When nodules form in the thyroid. Causes of Goiter Iodine Deficiency: Iodine is essential for the production of thyroid hormones; its deficiency is a major cause of goiter in many areas of the world. Autoimmune diseases: Hashimoto’s thyroiditis and Graves’ disease are often associated with goiter. Infections or inflammation: Thyroiditis can cause temporary swelling of the gland. Genetic factors: A family history of thyroid problems increases the risk of developing goiter. Symptoms of Goiter Physical Symptoms: Visible swelling or mass in the neck. Difficulty swallowing or breathing. Systemic Symptoms: Fatigue. Weight variations. Trembling hands. Heart rhythm disturbances. Goiter Diagnosis To diagnose goiter, the endocrinologist may use several diagnostic tools, including: Blood tests: To check levels of the hormones T3, T4 and TSH. Thyroid ultrasound: To evaluate the structure and presence of nodules. Fine needle aspiration: Used in suspected cases to analyze thyroid cells. Goiter Treatment Medications: Thyroid hormones or medications to reduce hormone production. Radioactive iodine therapy: Used to reduce the size of the thyroid gland. Surgery: In severe cases, such as large goiter or suspected thyroid cancer. Conclusion Goiter is a condition that requires specialized medical attention. Timely diagnosis and proper treatment help prevent complications. If you notice swelling in the neck or other symptoms, do not hesitate to consult an endocrinologist for a thorough evaluation. Together for a healthy future! Book your consultation with a specialist doctor now! Your Medical Clinic staff provides all patients with specialized medical service at the highest standards. (+355) 69 627 7162
The Collector and the Darkness Stones

The Collector and the Darkness Stones What Should You Know? The gallbladder is a small organ that plays an important role in digesting fats. Unfortunately, the formation of gallstones can cause severe pain and serious complications. In this blog, we will examine what gallstones are, what causes them to form, the symptoms, and available treatments. What Are Gallstones? Gallstones are solid formations that develop in the gallbladder. They are usually composed of cholesterol, bile salts, or bilirubin. Their size can vary from a few millimeters to several centimeters, causing different symptoms based on their size and location. Main Causes of Gallstones High-fat diets: High consumption of fatty foods increases the risk of stone formation. Genetic factors: A family history of this condition is an important risk factor. Age and gender: Women and people over 40 are more likely to develop gallstones. Symptoms of Gallstones Severe pain: Sharp sensation in the right side of the abdomen, especially after consuming fatty meals. Nausea and vomiting: These often occur during acute attacks. High fever and jaundice: These symptoms may indicate complications such as infections or bile duct obstructions. Diagnosis and Treatment Diagnosis Abdominal ultrasound: The most common method for detecting gallstones. CT or MRI: Used in more complex cases to evaluate the condition of the gallbladder and bile ducts. Treatment Medications: In mild cases, these are prescribed to help dissolve the stones. Laparoscopic Cholecystectomy: A safe and effective procedure, it is the most common treatment for stones that cause significant symptoms. Conclusion Gallstones are a common condition that can be successfully managed with lifestyle changes and appropriate medical treatment. Early diagnosis and targeted intervention are key to avoiding complications. If you suspect you have gallstones, see a gastroenterologist for professional advice and treatment. Take care of your health and don’t ignore the signs that may indicate gallbladder problems! Together for a healthy future! Book your consultation with a specialist doctor now! Your Medical Clinic staff provides all patients with specialized medical service at the highest standards. (+355) 69 627 7162
Hernia EN
Hernia: Types, Risks and Treatment A hernia is a common condition that occurs when an organ or tissue protrudes through a weak hole in the muscle, causing swelling and often pain. In this blog, we will look at the main types of hernias, the symptoms that accompany this condition, and the best ways to treat it. What is Hernia? A hernia appears as a visible bulge, usually in the abdominal or groin area. It can be congenital or acquired due to weakening of the muscles, caused by factors such as lifting heavy objects, pregnancy, or aging. Main Types of Hernia Inguinal hernia: The most common type, affecting mostly men. Umbilical hernia: This occurs around the belly button and is more common in newborns or women after pregnancy. Hiatal hernia: Occurs in the diaphragm, when the upper part of the stomach moves toward the chest. Femoral and incisional hernias: Less common, but still require special attention and treatment. Symptoms of Hernia Visible swelling: In the affected area, which becomes more noticeable when standing or coughing. Pain or burning sensation: Often occurs during physical exertion or strenuous activity. Feeling of heaviness: Especially after eating or standing for long periods. Hernia Treatment Diagnosis Physical examination: To identify swelling and tenderness in the affected area. Medical tests: Ultrasound, CT scan or MRI help to accurately assess the hernia and possible complications. Treatment Options Monitoring: Small hernias that do not cause symptoms are carefully monitored. Laparoscopic surgery: A modern and minimally invasive technique, very effective for hernia repair and reduction of recovery time. Conclusion Hernia is a condition that should not be underestimated, as it can lead to serious complications, such as intestinal obstruction or infection. Timely diagnosis and consultation with a surgeon are essential to prevent long-term consequences and ensure effective healing. If you suspect a hernia, do not hesitate to seek medical attention for the most appropriate treatment! Together for a healthy future! Book your consultation with a specialist doctor now! Your Medical Clinic staff provides all patients with specialized medical service at the highest standards. (+355) 69 627 7162

